Introduction to Technology
Neurorehabilitation has traditionally relied on physical therapy, pharmacological approaches, and invasive procedures to restore lost neural functions. However, recent advances in brain-computer interfaces (BCIs) are transforming this landscape, offering direct communication pathways between the brain and external devices. These innovations are not only enhancing recovery potential but also paving the way for personalized and adaptive therapeutic strategies.

What Are Brain-Computer Interfaces?
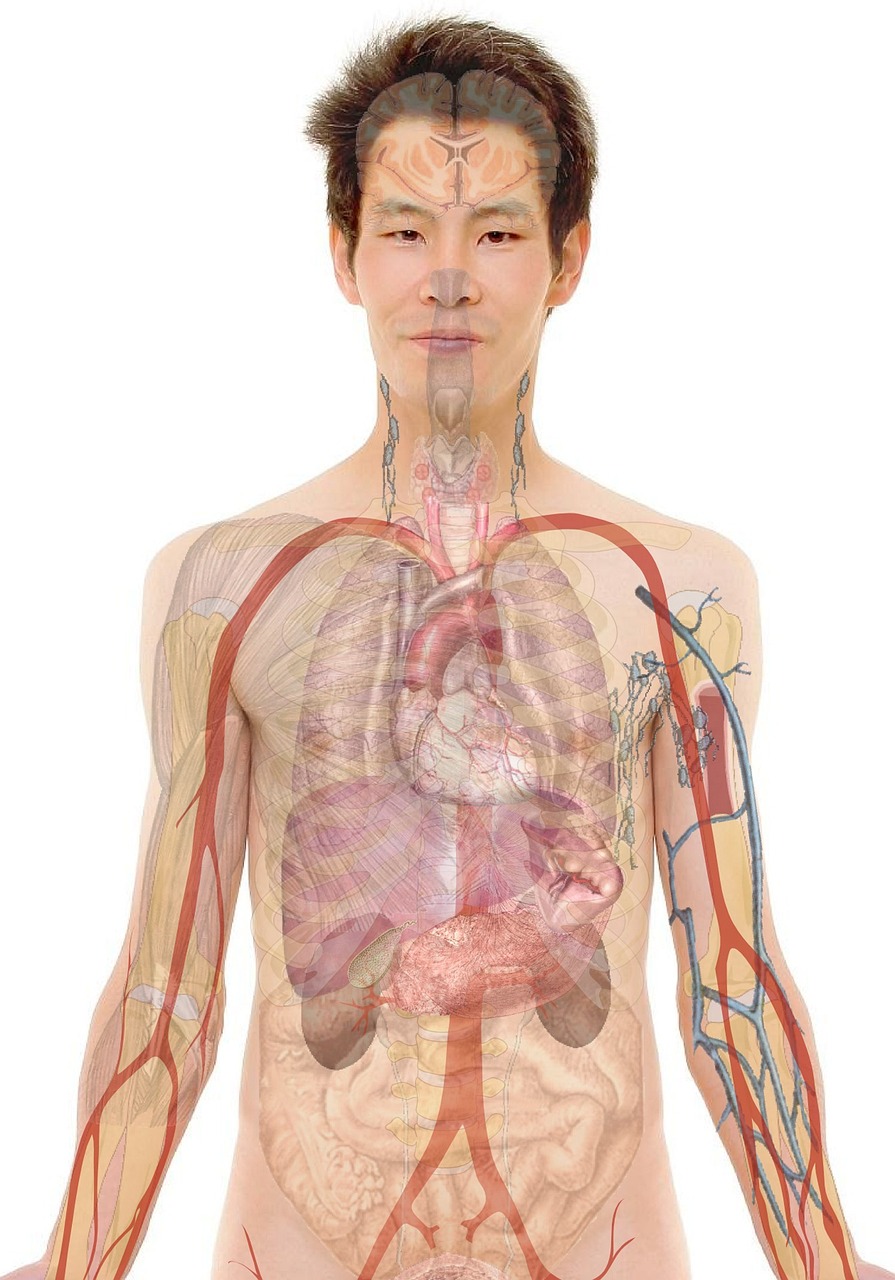
Brain-computer interfaces are systems that detect neural signals—often via electrodes implanted in or placed on the scalp—and translate them into commands to control external devices, such as robotic limbs, computer cursors, or functional electrical stimulation (FES) systems. By establishing a direct link between neural activity and machine output, BCIs bypass damaged neural pathways, offering new hope for individuals with neurological deficits.
Advancements in Neurorehabilitation Using BCIs
Restoring Motor Function
One of the most promising applications of BCIs is in restoring motor function for stroke survivors and individuals with spinal cord injuries. Systems utilizing decoded motor intentions allow patients to control prosthetic limbs or FES devices, promoting neural plasticity and encouraging reorganization of neural circuits involved in movement.
Enhancing Neural Plasticity
BCIs facilitate neuroplasticity— the brain's ability to reorganize itself—by providing real-time feedback. When patients see their neural activity translated into movement or other feedback cues, they can strengthen relevant neural pathways, leading to improved voluntary control over time.
Personalized Rehabilitation Protocols
Adaptive BCI systems customize therapy based on individual neural responses. This personalized approach ensures that interventions are tailored to the patient's unique neural architecture and progress, optimizing recovery trajectories.

Clinical Implementation and Challenges
Deploying BCIs in clinical settings involves overcoming challenges such as signal variability, device invasiveness, and user fatigue. Non-invasive options like EEG-based BCIs are more accessible but often less precise, while invasive approaches provide clearer signals but carry surgical risks. Striking a balance between efficacy and safety remains a focus of ongoing research.
The Future of BCIs in Neurorehabilitation
Future developments include integrating artificial intelligence for improved decoding accuracy, developing hybrid systems combining multiple neural signals, and expanding applications to cognitive and emotional rehabilitation. As technology advances, BCIs are poised to become standard tools in neurorehabilitation, offering dynamic, patient-centered care.
Conclusion
Brain-computer interfaces are revolutionizing neurorehabilitation by providing novel pathways for restoring lost functions, enhancing neuroplasticity, and tailoring therapies to individual needs. While challenges remain, the revolutionary potential of BCIs promises a future where recovery from neurological injuries is more effective, accessible, and personalized than ever before.