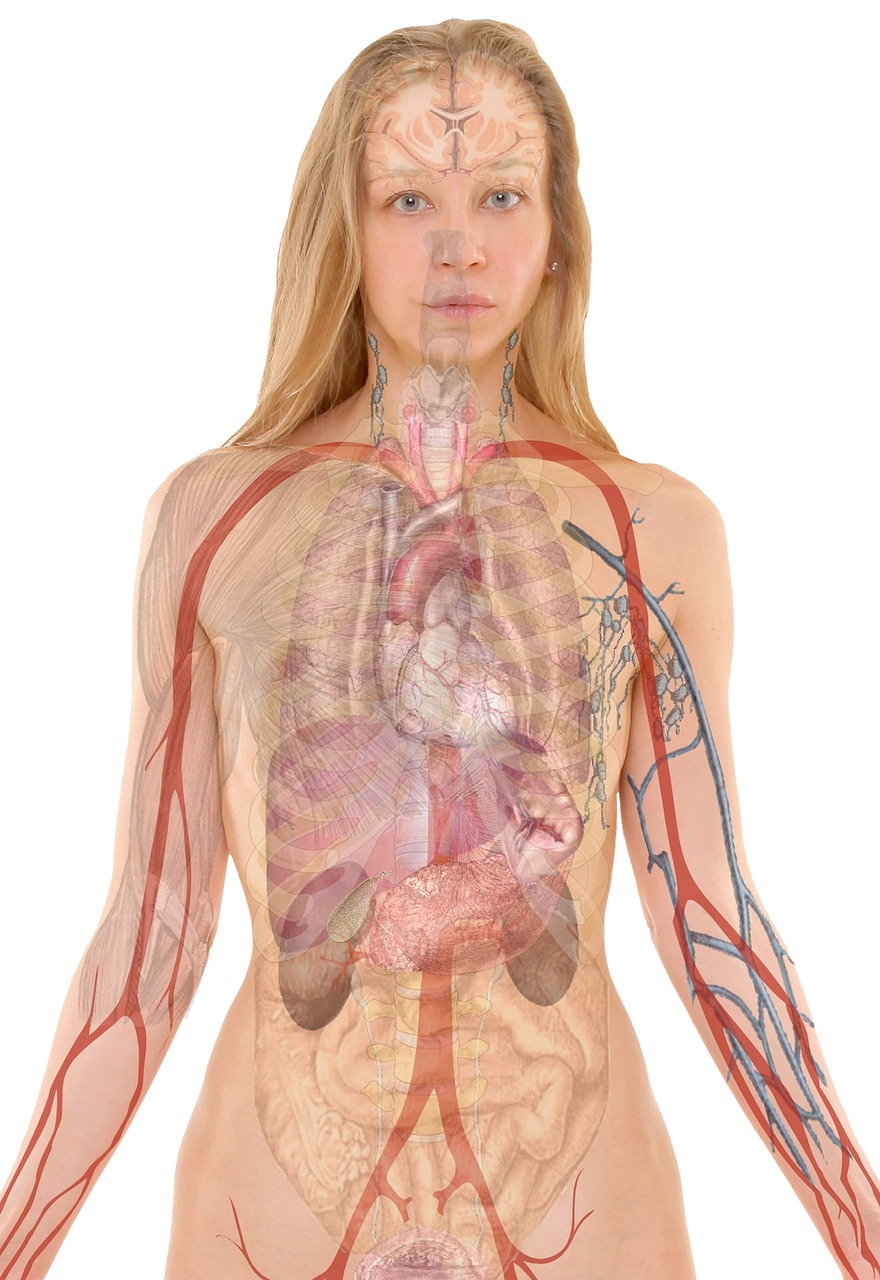
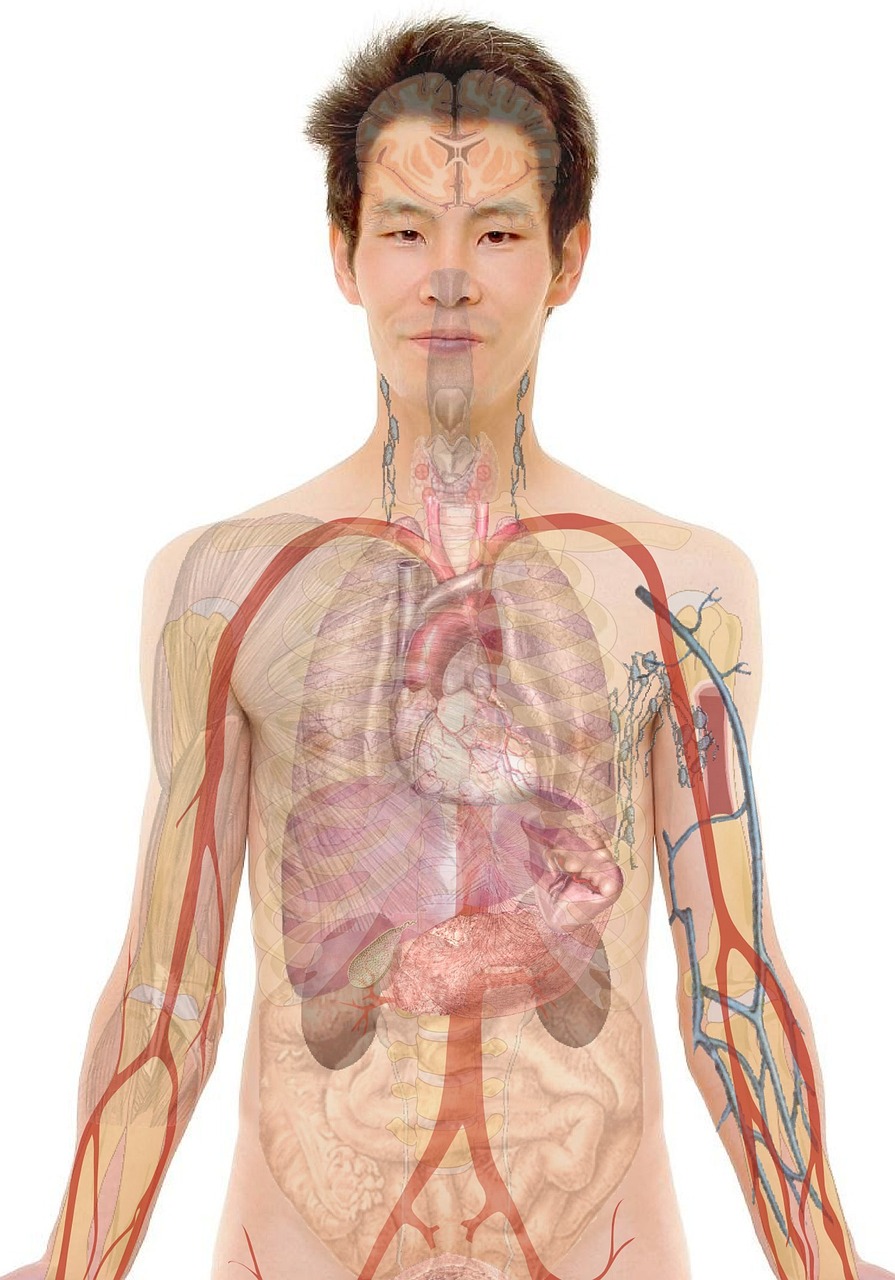
The human brain possesses an extraordinary capacity to record experiences, shaping our understanding of the world and guiding future actions. Yet, this remarkable ability takes a darker turn when faced with trauma. Traumatic events, by their very nature, are often burned into memory with excruciating detail and persistent intensity, frequently leading to debilitating conditions like Post-Traumatic Stress Disorder (PTSD). At the heart of this complex process lies the hippocampus, a seahorse-shaped structure deep within the temporal lobe, playing a pivotal role in the formation and consolidation of these indelible, and often unwelcome, memories.

Unraveling the Neurobiological Mechanisms of PTSD and Memory Persistence
Overview
The human brain possesses an extraordinary capacity to record experiences, yet this remarkable ability can become a source of profound suffering when confronted with trauma. Traumatic experiences often leave an indelible mark, leading to debilitating conditions like Post-Traumatic Stress Disorder (PTSD). At the heart of this complex phenomenon lies the hippocampus, a seahorse-shaped structure deep within the brain's temporal lobe, critically involved in memory formation and spatial navigation. Understanding how the brain consolidates traumatic memory, particularly the 'hippocampal echo' – the neural replay of past events – is paramount to developing effective interventions for PTSD. This article delves into the intricate neuroscience behind traumatic memory consolidation, exploring the roles of various brain regions, signaling molecules, and the dynamic interplay that solidifies fearful recollections.
Principles & Laws
The Dual Role of the Hippocampus
The hippocampus is a cornerstone of declarative memory, responsible for encoding new explicit memories (facts and events) and their initial temporary storage. During memory consolidation, a process where unstable new memories transform into stable long-term memories, the hippocampus acts as a critical hub. It facilitates the transfer of these memories to various cortical regions for more permanent storage, a process known as systems consolidation. A fascinating aspect of hippocampal function is neural replay, where sequences of neuronal activity corresponding to past experiences are reactivated, often at an accelerated pace, during quiet wakefulness or sleep. In the context of trauma, aberrant or persistent replay of traumatic events is hypothesized to contribute to their strong consolidation and intrusive nature.
The Amygdala and Fear Circuitry
While the hippocampus handles the 'what' and 'where' of a memory, the amygdala, an almond-shaped structure adjacent to the hippocampus, imbues it with emotional significance, particularly fear. The amygdala is central to fear conditioning and the storage of emotional memories. In traumatic experiences, the strong interaction between the hippocampus and amygdala is crucial. The hippocampus provides contextual information (where and when the trauma occurred), while the amygdala associates intense fear with that context, leading to robust fear memories. This intricate circuitry explains why reminders of a traumatic event can trigger intense emotional responses.
Stress Hormones and Memory Modulation
Acute stress during or immediately after a traumatic event floods the brain with stress hormones, primarily glucocorticoids (like cortisol) and catecholamines (like norepinephrine). These hormones profoundly influence memory formation and consolidation. While moderate levels of stress hormones can enhance memory for salient events – a survival mechanism – excessive or prolonged exposure can impair hippocampal function, leading to fragmented or distorted declarative memories, yet paradoxically strengthening emotionally charged, amygdala-dependent fear memories. This differential impact on different memory systems is key to understanding the distorted memory profiles observed in PTSD, where factual recall might be poor, but emotional reactions are vivid.
Synaptic Plasticity: Hebbian Principles
At the cellular level, the physical basis of memory lies in changes in synaptic strength, a phenomenon known as brain plasticity. Donald Hebb's seminal principle, "neurons that fire together wire together," describes how coincident activity in pre- and post-synaptic neurons strengthens their connection, leading to Long-Term Potentiation (LTP). Conversely, Long-Term Depression (LTD) weakens connections. Traumatic experiences are thought to induce powerful, sustained LTP in circuits connecting the hippocampus and amygdala, effectively 'hardwiring' the fear response to specific contexts or cues. Understanding these plasticity mechanisms is vital for developing targeted interventions.
Methods & Experiments
Human Neuroimaging
Advances in human neuroimaging have revolutionized our understanding of traumatic memory. Functional Magnetic Resonance Imaging (fMRI) allows researchers to observe patterns of brain activity and connectivity, revealing altered hippocampal activity and disrupted functional connectivity between the hippocampus, amygdala, and prefrontal cortex in individuals with PTSD. Electroencephalography (EEG) and Magnetoencephalography (MEG) provide insights into neural oscillations and event-related potentials, offering clues about the temporal dynamics of memory processing and potential aberrant neural replay.
Animal Models of Traumatic Memory
Pre-clinical research heavily relies on animal models, particularly rodents, to study the cellular and circuit mechanisms of traumatic memory. Fear conditioning paradigms, where an animal learns to associate a neutral stimulus (e.g., a tone or a context) with an aversive event (e.g., a mild foot shock), are widely used. These models allow precise manipulation of neural circuits and the study of behavioral assays like freezing responses, providing insights into the neurobiology of fear learning and extinction, and how traumatic memories are formed and maintained.
Optogenetics and Chemogenetics
These cutting-edge techniques enable unprecedented control over specific neural circuits. Optogenetics uses light to control genetically modified neurons, while chemogenetics uses engineered receptors activated by specific inert designer drugs. By selectively activating or inhibiting neurons within the hippocampus or amygdala, researchers can investigate the causal roles of these structures in memory consolidation and fear expression, offering a powerful tool to dissect the complex circuitry underlying traumatic memory.
Pharmacological Interventions
Experimental pharmacology plays a crucial role in identifying potential therapeutic targets. Researchers test drugs that modulate neurotransmitter systems (e.g., adrenergic, glutamatergic, GABAergic) or stress hormone pathways (e.g., beta-blockers, glucocorticoid receptor antagonists) to observe their effects on memory encoding, consolidation, and retrieval in both animal models and human trials.
Data & Results
Altered Hippocampal Function in PTSD
Consistent findings from neuroimaging studies show structural and functional alterations in the hippocampus of individuals with PTSD. These often include reduced hippocampal volume and altered patterns of activity – sometimes hyperactive during emotional processing, other times hypoactive during memory retrieval, suggesting a dysregulated system. Furthermore, disrupted functional connectivity between the hippocampus, the amygdala, and the prefrontal cortex is a hallmark, contributing to impaired emotional regulation and contextual processing.
Exaggerated Amygdala Activity
In PTSD, the amygdala frequently exhibits exaggerated responses to trauma-related cues, underpinning the enhanced fear responses and hypervigilance characteristic of the disorder. Critically, data suggest an impairment in fear extinction – the process by which fear responses diminish when a conditioned stimulus is repeatedly presented without the aversive outcome. This failure of extinction is a significant mechanism contributing to the persistence of traumatic memories.
Stress Hormone Effects
Research has demonstrated the complex effects of stress hormones. While moderate levels of cortisol can enhance initial emotional memory encoding, chronic or excessive stress can impair hippocampal neurogenesis and synaptic plasticity, hindering the precise contextual binding of memories. Paradoxically, this can lead to overgeneralization of fear, where non-threatening stimuli evoke fear responses, a common feature in PTSD. The timing of stress hormone release relative to the traumatic event and subsequent memory consolidation window is critical.
Neural Replay of Traumatic Events
Animal studies provide compelling evidence for the replay of fearful contexts during sleep, particularly in the hippocampus. This replay is thought to strengthen the neural circuits supporting the traumatic memory, facilitating its transfer to cortical storage and contributing to its enduring nature. Abnormal patterns of replay, perhaps more frequent or more intense, could contribute to the intrusive recollections experienced by individuals with PTSD.
Applications & Innovations
Targeting Memory Reconsolidation
One of the most promising avenues is targeting memory reconsolidation. When a consolidated memory is retrieved, it temporarily becomes labile again, entering a 'reconsolidation window' during which it can be modified or even weakened before being re-stored. Pharmacological interventions, such as administering beta-blockers (e.g., propranolol) during memory retrieval, aim to disrupt the strengthening of fear memories. Behavioral interventions, like extinction therapy performed within this reconsolidation window, can also be highly effective in weakening the emotional component of traumatic memory.
Fear Extinction Therapies
Exposure therapy, a form of fear extinction therapy, is a frontline treatment for PTSD. Innovations include virtual reality (VR) exposure therapy, which offers a controlled and customizable environment for patients to confront trauma-related cues safely. Research also explores augmenting extinction learning with pharmacological agents or cognitive strategies to enhance its effectiveness and reduce relapse.
Neuromodulation Techniques
Non-invasive neuromodulation techniques like Transcranial Magnetic Stimulation (TMS) are being explored to target specific brain regions involved in PTSD, such as the prefrontal cortex or amygdala, to modulate their activity and improve symptom severity. Deep Brain Stimulation (DBS), while more invasive, is a potential future direction for severe, treatment-resistant cases, by directly modulating dysfunctional neural circuits.
Personalized Medicine Approaches
Recognizing the heterogeneity of trauma responses, a personalized medicine approach is gaining traction. This involves using genetic markers, neuroimaging profiles, and biomarkers (e.g., specific stress hormones levels) to predict an individual's risk for PTSD, inform treatment selection, and tailor interventions for optimal efficacy.
Key Figures
- Donald Hebb: A pioneer in neurophysiology, whose concept of Hebbian learning ("neurons that fire together wire together") laid the groundwork for understanding brain plasticity and synaptic mechanisms of memory.
- Eric Kandel: Nobel laureate for his work on the molecular mechanisms of learning and memory in sea slugs (Aplysia), demonstrating how synaptic changes underpin memory formation (LTP and LTD).
- Joseph LeDoux: Renowned for his extensive research on the neural circuits of emotion, particularly the central role of the amygdala in fear learning and memory.
- Roger Pitman: A leading psychiatrist and researcher known for his work on PTSD, especially his pioneering studies on using propranolol to disrupt the reconsolidation of traumatic memories.
- Brenda Milner: Her seminal work with patient H.M. profoundly established the critical role of the hippocampus in forming new long-term declarative memories, setting the stage for modern memory research.
Ethical & Societal Impact
Memory Manipulation Ethics
The ability to modulate or erase traumatic memory raises profound ethical questions. Concerns include the potential for altering personal identity, the implications for legal testimonies where memories are crucial, and the risk of misuse if such technologies become widely available. Careful consideration of informed consent and societal oversight is paramount.
Stigma and Access to Care
Despite increased awareness, a significant stigma still surrounds mental health conditions like PTSD. Research in this area not only offers new treatments but also helps de-stigmatize the condition by grounding it in neurobiological mechanisms. Ensuring equitable access to advanced therapies, especially in underserved populations, remains a critical societal challenge.
Legal and Forensic Implications
Understanding the neurobiology of traumatic memory also has implications for the legal system. The fact that memories can be fragmented, enhanced, or distorted under stress raises questions about the reliability of eyewitness testimony and victim accounts in forensic contexts. Neuroscience can inform judicial understanding of memory processes.
Current Challenges
Heterogeneity of Trauma Responses
One of the biggest challenges in PTSD research is the vast heterogeneity in individual responses to trauma. Not everyone exposed to trauma develops PTSD, and symptoms vary widely. Identifying genetic predispositions, epigenetic markers, and individual differences in brain plasticity that confer vulnerability or resilience is crucial but complex.
Translational Gap
Despite significant advances in animal models, translating findings from rodents to complex human conditions remains a persistent challenge. The intricate interplay of human cognition, emotional regulation, and social factors adds layers of complexity that are difficult to replicate in controlled animal experiments.
Complex Brain Circuitry
Traumatic memory involves a dynamic, widespread network of brain regions, including the hippocampus, amygdala, prefrontal cortex, insula, and others. Disentangling the precise contributions and interactions of these regions, and understanding how they become dysregulated in PTSD, requires sophisticated multi-modal approaches.
Treatment Resistance
A significant portion of individuals with PTSD do not respond adequately to current treatments, highlighting the need for novel therapeutic strategies. Overcoming this resistance requires a deeper understanding of the underlying neurobiology and personalized approaches.
Future Directions
Precision Neuroscience
The future of traumatic memory research lies in precision neuroscience. This involves leveraging advanced analytics, including Artificial Intelligence (AI) and machine learning, to integrate genetic data, neuroimaging, psychophysiological measures, and clinical profiles. The goal is to develop highly individualized treatment plans based on a patient's unique neurobiological signature, predicting which interventions will be most effective.
Early Intervention Strategies
Identifying reliable biomarkers for PTSD risk immediately following trauma could enable proactive, early intervention strategies. These might include pharmacological agents to modulate memory consolidation during the acute post-trauma phase or targeted psychological interventions designed to prevent the persistent "hippocampal echo" from solidifying into full-blown PTSD.
Advanced Neuroimaging and AI
Real-time neurofeedback, guided by fMRI or EEG, could allow individuals to learn to modulate their own brain activity in regions like the amygdala or hippocampus, potentially enhancing emotional regulation and memory processing. Combining this with AI-driven predictive models could refine therapeutic protocols. Furthermore, the use of virtual reality (VR) and augmented reality (AR) in exposure therapy is rapidly advancing, offering highly immersive and customizable environments for therapeutic interventions.
Understanding Resilience
Shifting focus from pathology to resilience is another critical future direction. Studying individuals who are exposed to trauma but do not develop PTSD can reveal protective neurobiological mechanisms and genetic factors that foster adaptive brain plasticity. These insights could inform strategies to enhance resilience in vulnerable populations.
Conclusion
The hippocampus stands as a central figure in the intricate drama of traumatic memory consolidation. Its dynamic interplay with the amygdala, modulated by stress hormones and shaped by brain plasticity, dictates whether a traumatic experience fades or becomes an enduring source of suffering. Through meticulous neuroscience research employing cutting-edge methodologies, we are steadily decoding the 'hippocampal echo' and its profound implications for PTSD. While significant challenges remain, the burgeoning understanding of these mechanisms offers immense hope for developing innovative and personalized treatments that can alleviate the burden of traumatic memories, ultimately enhancing human well-being and fostering resilience in the face of adversity.